The International Diabetes Federation (IDF) and International Agency for the Prevention of Blindness (IAPB) have called for integration of diabetic retinopathy care into all diabetes policies and national health strategic plans to prevent vision impairment and blindness.
Mr Peter Holland, Chief Executive, IAPB, made the call during an online meeting and launch of a joint policy brief on “Diabetic retinopathy: a call for global action” on Tuesday.
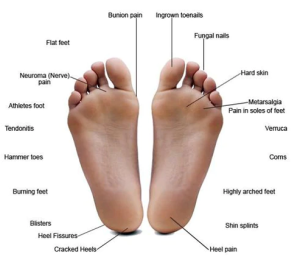
Diabetes is a metabolic disorder characterised by high blood glucose (sugar) levels.
Diabetic Retinopathy (DR) is a chronic progressive disease of the retinal capillaries (small blood vessels) associated with prolonged raised blood glucose levels in people with diabetes.

Holland noted that diabetes is now recognised as a global epidemic with diabetic retinopathy being one of the feared complications of most people living with diabetes.
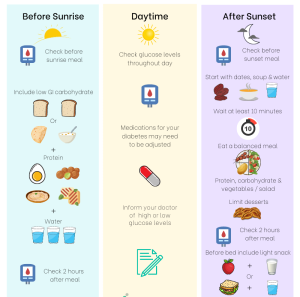
“All people with diabetes are at risk of developing DR, although those with poor blood glucose and blood pressure management and hyperlipidaemia are most at risk.
“That’s why this collaboration is important.
“We are advocating for improved diabetes care and regular retinal screening made available and accessible for every individual living with diabetes,” he said.
According to him, early detection can lead to timely treatment of DR, which can prevent 95 per cent of vision impairment and blindness.

Holland emphasised that a multisectoral response was crucial, not only to address the causes of diabetes and DR, but also to prevent vision loss caused by DR.
He said that national strategies for DR must be integrated and aligned with national diabetes programmes.
According to him, close collaboration and co-management of people with diabetes involving dietitians, endocrinologists, family medicine specialists, primary eye care providers and ophthalmologists are essential.
Also, Prof. Akhtar Hussain, President, IDF, said that diabetes and diabetic retinopathy are growing concerns that posed significant challenges to the health, social and economic development of millions of people.
Hussain noted that globally, 537 million adults aged 20 to 79 years are living with diabetes, a number that was predicted to reach 1.3 billion in 50 years.
According to him, the high prevalence of type 2 diabetes continues to rise worldwide and is particularly rapid in low-and middle-income countries.
“In these settings, there is limited availability and affordability of healthcare services for screening and treating diabetes-related complications, such as retinopathy, to prevent vision loss,” he said.
Similarly, Dr Bente Mikkelsen, Director, Non-Communicable Diseases Department, World Health Organisation (WHO), urged countries to implement integrated people-centred eye care, including preventable vision impairment and blindness in health systems.

Mikkelsen called for strengthened health promotion and prevention for diabetes and DR, and improved affordability and access to DR treatment including technology and medicines.
Commenting, Dr Covadonga Bascaran, Clinical Research Fellow, International Centre for Eye Health, London School of Hygiene & Tropical Medicine, said DR was the leading cause of blindness that increased globally in age standardised prevalence between 1990 and 2020.
Bascaran noted that estimated global prevalence of DR among people with diabetes was approximately 22 per cent, with variations between countries.
According to her, high-income countries tend to diagnose diabetes earlier, compared to resource constrained settings where diabetes diagnosis was often made when complications have already occurred.
Bascaran stressed the need to take action to address DR as one of the most common diabetes complications that could greatly affect the quality of life of people with diabetes.
IDF Blue Circle Voice member from Nigeria, Chimezie Anyiam, said she was diagnosed with type 2 diabetes in January 2013 at the age of 26 years and with diabetic retinopathy seven years later in February 2020.
“I learnt my eyesight was affected by my high blood glucose levels due to poor management.
“I don’t recall receiving any information on living with diabetic retinopathy at the time of my diagnosis. However, my life did change.
“I had regular eye examinations and managed my blood sugar regularly to prevent my eyesight from worsening. I use prescription eye drops, which at times have been challenging to access.
“I want my government to improve the prevention and treatment of type 2 diabetes and diabetic retinopathy and to improve the quality of life of people living with these conditions.
“Unfortunately, I regret to say I have very little hope that my government feels concerned enough to address these issues,” she said. (NAN)


