Scientists at the University of Oxford have begun the human testing of an experimental vaccine against the brain-swelling Nipah virus that led to outbreaks in India’s Kerala state and other parts of Asia.
This is the first in-human trial of the ChAdOx1 NipahB vaccine, being developed by researchers at the institution’s Pandemic Sciences Institute.
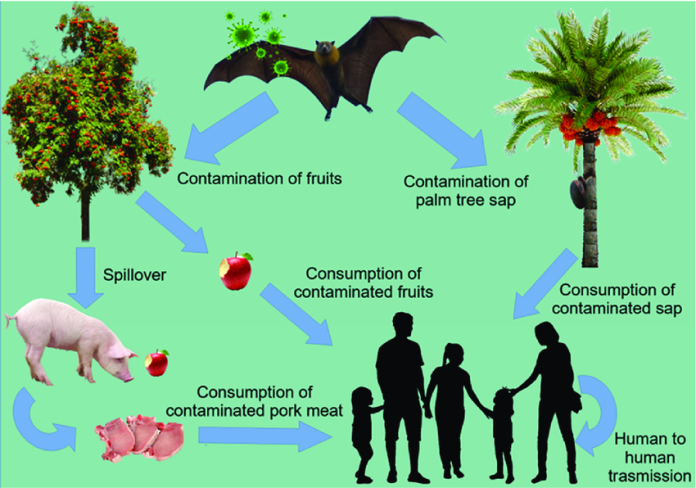
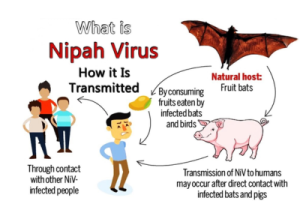
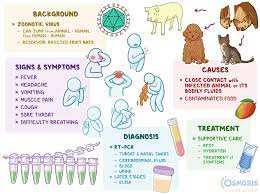
Nipah virus infection is a zoonotic illness that is transmitted to people from animals, and can also be transmitted through contaminated food or directly from person-to-person.
The World Health Organisation says the virus causes a range of illnesses from asymptomatic (subclinical) infection to acute respiratory illness and fatal encephalitis in infected people.
It said the virus can also cause severe disease in animals such as pigs, resulting in significant economic losses for farmers.
Although Nipah virus has caused only a few known outbreaks in Asia, it infects a wide range of animals and causes severe disease and death in people.
 According to the Oxford Vaccine Group, 51 people aged 18 to 55 will participate in the trial, which is being led by the OVG within the Department for Paediatrics, and funded by the Coalition for Epidemic Preparedness Innovations.
According to the Oxford Vaccine Group, 51 people aged 18 to 55 will participate in the trial, which is being led by the OVG within the Department for Paediatrics, and funded by the Coalition for Epidemic Preparedness Innovations.
The trial’s Principal Investigator and Professor of Infectious Diseases at the Centre for Clinical Tropical Medicine and Global Health, Prof. Brian Angus, said: “Nipah virus was first identified in 1998; yet, 25 years on, the global health community still has no approved vaccines or treatments for this devastating disease.
“Due to the high mortality rate and the nature of Nipah virus transmission, the disease is identified as a priority pandemic pathogen.
“This vaccine trial is an important milestone in identifying a solution that could prevent local outbreaks occurring, while also helping the world prepare for a future global pandemic.”
The Acting Executive Director of Vaccine Research & Development at CEPI, one of the leading global funders of Nipah virus research, Dr In-Kyu Yoon, said, “Nipah has epidemic potential, with its fruit bat hosts found in areas home to over two billion people.
“This trial is a step forward in efforts to build a suite of tools to protect against this killer virus. Knowledge gained could also inform development of other Paramyxovirus countermeasures.”
 Meanwhile, it has been projected that the vaccine trial will run over the next 18 months, with further trials expected to follow in a Nipah-affected country.
Meanwhile, it has been projected that the vaccine trial will run over the next 18 months, with further trials expected to follow in a Nipah-affected country.
Nipah virus has caused only a few known outbreaks in Asia.
The global health body noted that during the first recognised outbreak in Malaysia, which also affected Singapore, most human infections resulted from direct contact with sick pigs or their contaminated tissues.
“In subsequent outbreaks in Bangladesh and India, consumption of fruits or fruit products (such as raw date palm juice) contaminated with urine or saliva from infected fruit bats was the most likely source of infection.
Human-to-human transmission of Nipah virus has also been reported among family and care givers of infected patients,” it added.