For many people living in the 21st Century, the tern ‘scleroderma’ seems alien. Yet, this condition has silently persisted since the 18th and 19th centuries when it was first recognized as a rare, chronic autoimmune skin disorder.
The word itself is a fusion of Greek roots with “sclero” meaning hard and “derma” meaning skin, aptly describing the disease’s hallmark symptom of skin hardening.
 Understanding scleroderma
Understanding scleroderma
It is a systemic sclerosis, a chronic autoimmune ailment where the body’s immune’s system turns against itself. The name, “scleroderma” reflects one of the most visible signs of the disease: the hardening of the skin.
However, this condition doesn’t stop at the skin’s surface; it often infiltrates vital organs such as the lungs, heart, gastrointestinal system, tendons, and joints, making it potentially life-threatening.
It’s also crucial to note that scleroderma is neither contagious nor infectious, and it certainly isn’t a form of cancer.
Statistics also reveal that about 80 percent of those diagnosed with the systemic sclerosis are women. In the United States alone, an estimated 300,000 to 700,000 individuals grapple with this condition; while globally, around 2.5 million people face the challenge.
Although Scleroderma typically strikes individuals between the ages of 25 and 55, it can appear at nearly any age. Approximately, one-third of patients experience the systemic form of the disease.
Faces of scleroderma

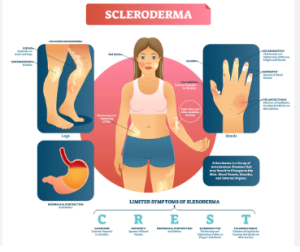
According to rheumatologists, scleroderma presents itself in several distinct forms, each with its unique features and hitches.
Localized scleroderma: primarily affects the skin, resulting in patchy, often sticky changes that don’t distress internal organs, except possibly the esophagus.
Systemic scleroderma: is the more extensive form, impacting not only the skin, but also the joints, heart, lungs, gastrointestinal tract, kidneys, bladder, nerves, muscles, blood vessels and joints; and manifests in two primary patterns: organ hardening and fibrosis.
Diffuse scleroderma: has variant features with rapid skin thickening, affecting more skin than the limited form. Its victims face a higher risk of internal organ involvement compared to those with the limited form.
Limited scleroderma: its skin thickening is less widespread and typically confined to the face, distal arms, hands, legs and feet; while the internal organs may still be affected, its involvement is less frequent and severe than in diffuse scleroderma.
Impact on the body
Scleroderma’s effects vary significantly from person-to-person, as some individuals experience only skin-related issues, while others grapple with hidden complications in their internal organs.

One common symptom, Raynaud’s phenomenon, affects roughly 90 to 95 percent of patients, as it results from the constriction of blood vessels, causing fingers and toes to turn white – due to decreased blood flow; then blue – due to oxygen deprivation; and finally red – as blood vessels reflexively open.
Skin thickening, which gives scleroderma its name, results from inflammation and fibrosis. This can lead to tough, hardened skin, which presents physical and emotional challenges to patients.
Ulcerations are a common feature in the systemic form of the disease, resulting in slow-healing skin sores that can appear on the knuckles, elbows, toes or other areas.
scleroderma doesn’t stop at the skin’s surface; it often infiltrates vital organs such as the lungs, heart, gastrointestinal system, tendons, and joints, making it potentially life-threatening
Rheumatologists note that calcinosis deposits are painful hard lumps that may develop in or under the skin, causing considerable discomfort.
Telangiesctasia refers to dilated small blood vessels near the skin’s surface, appearing as small red spots, typically on the fingers, palms, face and lips.
Musculoskeletal involvement often leads to swelling or puffiness in the hands, a symptom that usually appears early in the disease. It can make the fingers feel swollen and stiff, making it difficult to form a fist.
Lung complications are another challenge, as inflammation and fibrosis hinder the transfer of oxygen from the air into the bloodstream, resulting in shortness of breath, exercise difficulties, and coughing, sometimes, leading to Interstitial Lung Disease (ILD), and pulmonary hypertension.
Heart involvement may cause palpitations and fluid retention in the legs, although it rarely causes severe symptoms. Kidney issues can range from mild to very serious, with easy signs including mild high blood pressure and abnormal blood rest results, potentially progressing to renal crisis, making it a dangerous condition resulting from rapid blood vessel damage in the kidneys.
Lastly, Scleroderma can disrupt the gastrointestinal tract, leading to issues in the esophagus, stomach and bowels. Fibrosis can develop in the gastrointestinal muscles, causing abnormal movement and hindering nutrient absorption.


